Medicare Advantage Prescription Drug Coverage
CareFirst BlueCross BlueShield Medicare Advantage provides comprehensive prescription drug coverage with NO annual deductible.
Are you eligible for Medicare through Medicaid?
2021 Dual Prime Plan (HMO D-SNP) Pharmacy Resources
Pharmacy resource information for our Dual Prime (HMO D-SNP) plan can be found here.
Search for Your Prescriptions
Find out if your prescription is covered.
Core Plan
Search for Your PrescriptionsEnhanced Plan
Search for Your Prescriptions30-day supply cost tier:
| CareFirst BlueCross BlueShield Advantage Core (HMO) | CareFirst BlueCross BlueShield Advantage Enhanced (HMO) | |
|---|---|---|
| Retail Pharmacy | Copay for 30-day Supply | Copay for 30-day Supply |
| Tier 1 - Preferred Generic | $7.00 | $5.00 |
| Tier 2 - Generic | $20.00 | $15.00 |
| Tier 3 - Preferred Brand | $47.00 | $47.00 |
| Tier 4 - Non-Preferred Drug | $100.00 | $100.00 |
| Tier 5 - Specialty | 33% of the total cost | 33% of the total cost |
For more on prescription drug costs, including prescription limitations and prior authorization requirements, see Chapters 5 and 6 of the Evidence of Coverage - Core or Evidence of Coverage - Enhanced.
 Our Pharmacy Network
Our Pharmacy Network
You’ll have access to over 65,000 pharmacies nationwide.
Most major pharmacy chains and many independent pharmacies are part of our network, including CVS, Walmart, Sam’s Club, Walgreens, Rite Aid, Sav-On Pharmacy, Safeway, Medicine Shoppe, Publix, Albertson’s, Costco, Kroger, Harris Teeter, Giant and Giant Eagle.
Most residents of our service area live within two miles of a participating pharmacy, making refills even more convenient.
 Sign Up for Mail Order Prescriptions and Save
Sign Up for Mail Order Prescriptions and Save
Save money and time by refilling prescriptions online, by phone or through email with CVS Caremark Mail Service Pharmacy. Choose your delivery location and consult with pharmacists by phone 24/7. Sign up for a 90-day supply by mail, and you’ll only pay the cost of a 60-day supply. (Tier 5- Specialty drugs are not eligible for 60-day and 90-day supplies via mail order. Please refer to the Evidence of Coverage - Core or Evidence of Coverage - Enhanced for more information.)
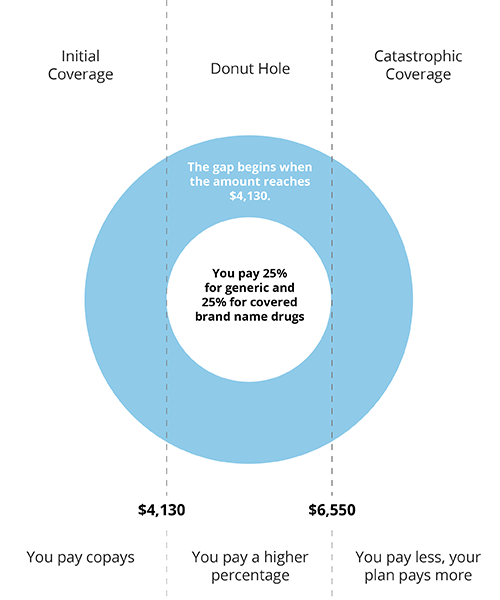
What is the donut hole or coverage gap?
The donut hole, or coverage gap, starts when your total drug costs—including what you and your plan have paid for drugs—reaches $4,130 for the calendar year. When you enter the donut hole, the amount you pay for your prescriptions will increase. Because of this, you are eligible for discounts to help you pay for your drugs. You will pay 25% for generics drugs and 25% for brand name drugs, plus a portion of the dispensing fee. Discounts vary depending on the drug and your plan’s Formulary
Our Enhanced Plan has special coverage for Tier 1 (Preferred Generic) in the donut hole or coverage gap:
The CareFirst BlueCross BlueShield Advantage Enhanced plan includes gap coverage for Tier 1 drugs (preferred generic) at the same mail, retail, out-of-network (OON) and long-term care (LTC) cost-sharing as shown below. For more information please refer to your Evidence of Coverage - Core or Evidence of Coverage - Enhanced.
| Tier 1 (Preferred Generic) |
Retail | Mail Order | Out-of-Network | Long Term Care |
|---|---|---|---|---|
| 30-Day | $5.00 | $5.00 | $5.00 | $5.00 (31-day) |
| 60-Day | $10.00 | $10.00 | Not Covered | Not Covered |
| 90-Day | $15.00 | $10.00 | Not Covered | Not Covered |